Adolescent Weight Loss Surgery
Adolescence is a crucial time in development, and today many young people are facing serious health risks due to obesity. In the United States, over one-third of adolescents aged 12 to 19 are considered overweight or obese, with rates continuing to rise. This epidemic not only has short-term effects on physical and mental health but long-term consequences as well. Here, we explore why adolescent obesity is such a growing concern, its potential causes and effects, and discuss possible solutions for curbing this growing health problem.
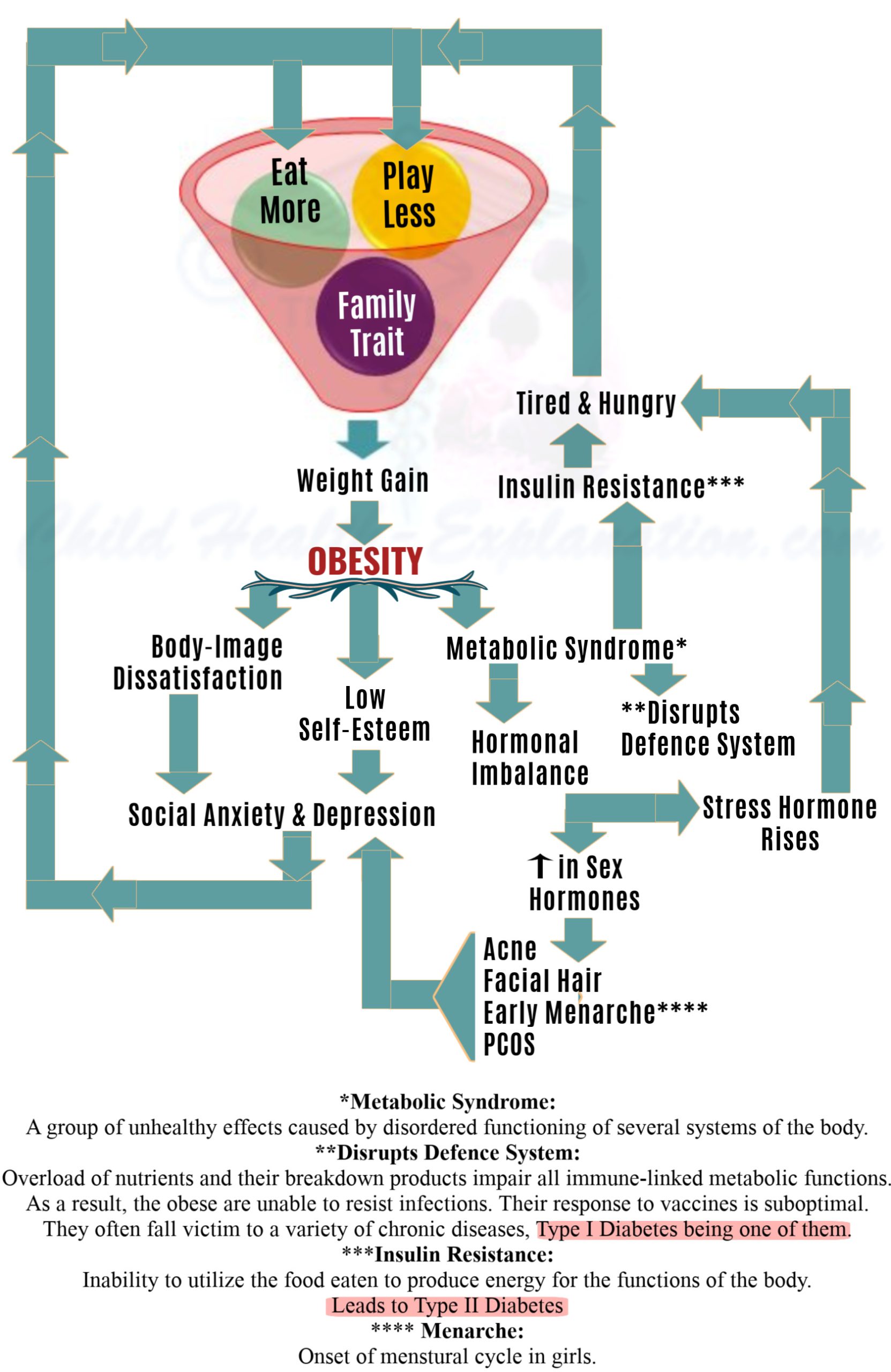
Adolescent Obesity Causes
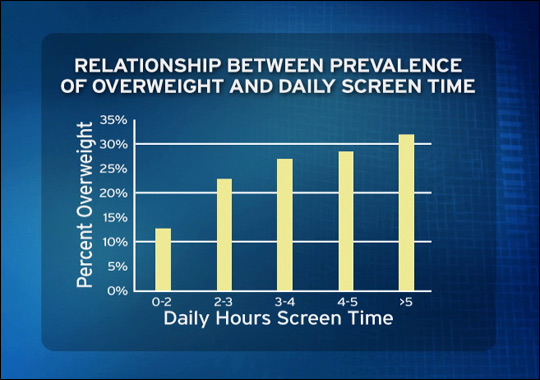
There is no single cause of adolescent obesity; it results from a complex combination of factors. Poor nutrition is a major contributor, with many children consuming diets high in processed foods, sugar, and saturated fats. A sedentary lifestyle can also be problematic; adolescents who spend much time on screens or in front of the television are less likely to participate in regular physical activity. Other potential causes include genetics, emotional eating, hormone imbalances, and socioeconomic.
Solutions To Combat Adolescent Obesity
To effectively address the issue of adolescent obesity, there must be changes at both an individual and societal level. Parents can encourage healthy eating habits by providing nutritious meals and snacks and limiting snacking and sugary beverages. Adolescents should get at least 60 minutes of moderate to vigorous physical activity daily and participate in recreational sports teams or classes. Schools can help by providing healthier lunch options and physical education classes focusing on fitness and nutrition. Finally, the government can promote awareness and create public policies that support healthier lifestyles.
Adolescent obesity is an urgent public health concern that requires attention from all levels of society to be successfully addressed. Parents, educators, healthcare providers, and governmental organizations must work together to create a supportive environment that encourages healthy eating patterns and regular physical activity. This will help reduce individual risk for chronic illnesses and lead to long-term improvements in overall public health.
Treating Adolescent Obesity
When treating childhood obesity, a comprehensive approach is the most effective. Behavioral and lifestyle changes, pharmacotherapy, and bariatric surgery may be necessary to reach a healthy weight for children with severe obesity (a body mass index above 120% of the 95th percentile).
Behavioral and lifestyle changes involve actively encouraging physical activity, reducing sedentary activities such as watching TV or playing video games, and instilling healthy eating habits. This can include reducing portion sizes, limiting unhealthy snacks and fast food, and increasing the consumption of nutritious meals that contain lean proteins, whole grains, fruits, vegetables, and low-fat dairy products. Cognitive-behavioral therapies can also help address emotional issues related to overeating.
Pharmacotherapy involves using medications under the supervision of the child’s physician. These medications are designed to reduce hunger, enhance metabolic rate and reduce caloric absorption.
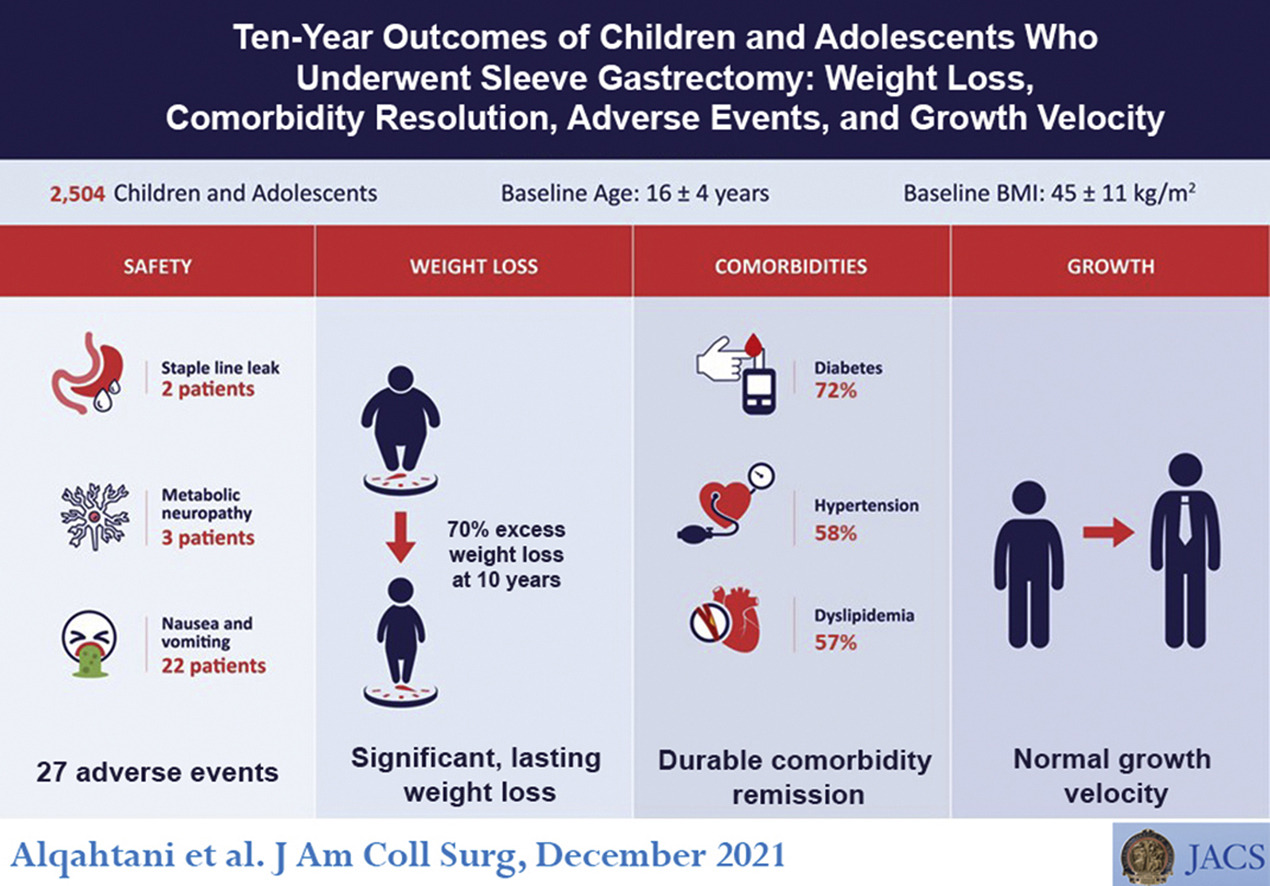
Metabolic and bariatric surgery is considered the most effective solution for adolescents and children with severe obesity. Research suggests that it leads to prolonged weight loss, improved quality of life, and alleviates associated health concerns such as type 2 diabetes, high blood pressure, sleep apnea, and premature death. Laparoscopic Roux-en-Y gastric bypass (RYGB) and laparoscopic vertical sleeve gastrectomy (VSG) are two approaches commonly used in pediatric cases.
Team Approach to Adolescent Bariatric Surgery
For children with severe obesity to receive the most effective and comprehensive medical care, a team approach is essential. This specialized team should include:
- a bariatric surgeon
- a pediatrician or internist with special expertise in endocrinology, gastroenterology, nutrition, and adolescent health
- a registered dietician who is knowledgeable in treating obesity and working with kids and their families
- a mental health professional trained in treating eating disorders and evaluating patients for bariatric surgery
- a nurse, social worker, or another individual to coordinate the evaluation and aftercare of patients
- an exercise specialist in providing safe physical activity recommendations.
By forming a multifaceted team, these professionals can collaborate on finding the best treatment plan and providing tailored patient education and support.
Obesity-related Health Problems
The effects of adolescent obesity reach far beyond weight gain. These young people are more likely to develop:
- chronic illnesses like diabetes
- heart disease
- mental health issues such as depression and low self-esteem
Obese adolescents are more likely to be bullied or face other forms of social discrimination. They may also experience difficulty sleeping and lower academic performance due to a lack of energy or concentration.
Type 2 Diabetes Mellitus (T2DM)
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disorder, primarily associated with obesity, that often develops later in life. In individuals with T2DM, the body’s tissues are not as sensitive to insulin, leading to high insulin and high sugar levels. Some children and adolescents affected by obesity develop T2DM early, leading to complications such as high blood pressure, high cholesterol, and liver disease, as well as long-term effects like heart disease, kidney failure, vision loss, and increased mortality. Fortunately, bariatric surgery has been shown to significantly improve or even eradicate T2DM in many adolescents who undergo it.
Non-alcoholic Fatty Liver Disease And Non-alcoholic Steatohepatitis
In addition to T2DM, another condition associated with childhood obesity is non-alcoholic fatty liver disease (NAFLD). This condition describes fat build up in the liver, seen in approximately 38% of children and adolescents affected by obesity, compared to just 5% of normal-weight individuals. Approximately 9% of those affected may also experience steatohepatitis, an inflammation of the liver, versus 1% of lean children and adolescents. Studies have found that NAFLD and steatohepatitis may cause liver damage, including cirrhosis, fibrosis, and scarring, but evidence suggests that bariatric surgery in adolescents can significantly reduce these conditions.
Cardiovascular Disease
Research into cardiovascular risk factors in children with obesity has revealed that they may be more likely to develop cardiovascular diseases in adulthood. Fortunately, research indicates that weight loss resulting from bariatric surgery may help to improve numerous cardiovascular risk factors in adults. Still, further research is necessary to understand the full effects on children and adolescents.
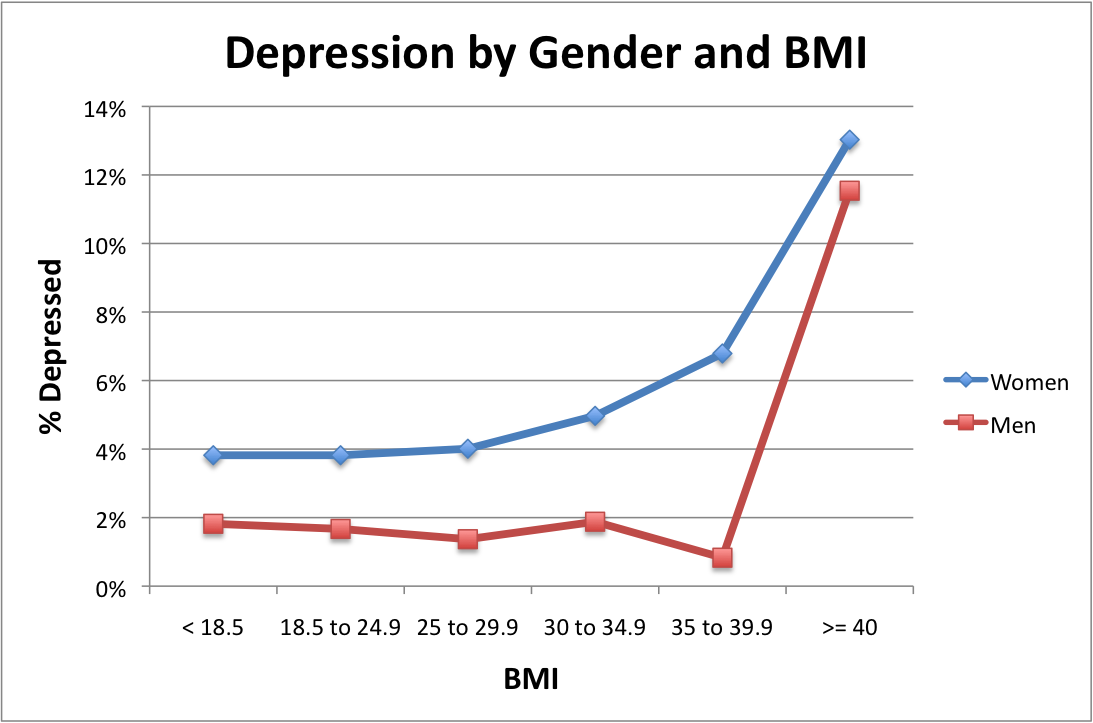
Teen Depression
Depression is a common problem among children and adolescents affected by obesity. While there isn’t much evidence that this condition worsens after bariatric surgery, the evidence indicates that it improves in adolescents who receive the treatment. However, adults may have a slightly increased risk for suicide following bariatric surgery. To combat this potential side effect, it is important that any pre-existing depression is treated and stable before undergoing surgery and monitored closely for signs of depression afterward.
Obstructive Sleep Apnea
Up to 22% of children with obesity have been found to have obstructive sleep apnea (OSA), which causes loud snoring or pauses in breathing during sleep, seen with fatigue and difficulty focusing at school. While tonsillectomies may help to treat OSA in some cases, if obesity is not addressed, symptoms will likely persist. Bariatric surgery may benefit those affected – studies have found that obstructive sleep apnea is improved or resolved in many post-surgery patients after their obesity is addressed.
Idiopathic Intracranial Hypertension
Idiopathic intracranial hypertension (IIH), formerly pseudotumor cerebri, is a medical condition characterized by headaches, visual changes, ringing in the ears, nausea, and vomiting caused by increased pressure inside the skull. Though the exact cause of IIH remains unknown, it has been linked to obesity. Fortunately, research suggests that symptoms frequently improve after months of bariatric surgery.
Quality Of Life
Children and adolescents with obesity often report a negative impact on their quality of life due to teasing, bullying, or the physical challenge of carrying extra weight. Thankfully, numerous studies have shown marked improvements in quality of life after receiving metabolic or bariatric surgery.
Eating Disorders
Though there is limited data available on the effects of bariatric surgery on teens with eating disorders such as bulimia nervosa, it is clear that they must be stable and receive treatment before receiving any kind of surgical intervention. With careful monitoring after surgery, the procedure can still provide positive results.
Bariatric Surgery for Adolescent Obesity
The ASMBS Public Education Committee and the ASMBS Pediatric Committee point out that recent research has demonstrated that adolescent bariatric surgery is as safe and effective as for adults. Several different metabolic and bariatric procedures exist, many of which are performed in children and teens. When deciding which procedure is most beneficial for a particular patient, a comprehensive evaluation must consider the surgical team’s expertise alongside feedback from the child and their family. Ultimately, choosing the right kind of bariatric surgery is an incredibly complex process that can yield positive results when properly managed.