Considering Weight Loss Surgery?
Obesity is a chronic and progressive disease that can affect multiple organs in the body. People with clinically severe obesity are at great medical risk of disability or premature death. In fact, four hundred thousand Americans die prematurely each year of obesity-related complications or co-morbidities.
At the top of the list of obesity-related co-morbidities are adult-onset diabetes, or Type 2 diabetes, and high blood pressure. High blood pressure caused by clinically severe obesity can contribute to heart attacks, congestive heart failure, and stroke. Health concerns such as sleep apnea, asthma, low-back pain, urinary stress incontinence, and severe acid reflux (GERD) are also a result of increased weight. Significant weight loss can often ease these conditions or reverse them completely.
What are the criteria for patients considering surgery for obesity or bariatric surgery?
Obesity is very difficult to treat. Many patients have tried multiple diets, medications, and exercise regimes that have had disappointing results. Surgery to promote weight loss by restricting food intake and interrupting the digestive processes is an option for clinically severe obese patients that have been unsuccessful with other weight loss treatments.
Eligible patients for weight loss surgery often have a body mass index (BMI) of at least 40 or greater or have a BMI of at least 35 with comorbid conditions associated with their obesity. A BMI of 40 generally translates to about 100 pounds over the ideal body weight for men or 80 pounds over the ideal body weight for women. Most patients don’t realize how overweight they truly are and need to check their ideal body weights and their BMI with a BMI calculator. For example, someone 5 feet 5 inches tall who weighs 209 pounds has a BMI of 35 and is technically about 75 pounds overweight.
Weight loss surgery may also be an option for people with a BMI of 35 or greater who suffer from significant obesity-related health problems such as diabetes, obesity-related heart disease, sleep apnea, or other diseases secondary to their weight. However, as is true for other treatments for obesity, successful results depend on a willingness to change one’s lifestyle.
There are patients who we may feel are good candidates for surgery based on their history of failed weight loss attempts and existing or impending medical conditions related to their weight but who have a BMI less than 35.
Introduction to Sleeve Gastrectomy
The sleeve gastrectomy is a surgery only on the stomach (it is a restrictive procedure) and does not involve any surgery on the intestine (which would make it malabsorptive). Sleeve gastrectomy has also been called partial gastrectomy and vertical sleeve gastrectomy. It basically consists of making a stomach that initially looks like a pouch into a long tube; therefore, the name “sleeve.” The sleeve gastrectomy (SG) removes about two-thirds of the stomach, which provides for quicker satiety (sense of fullness) and decreased appetite. The smaller stomach pouch restricts food intake by allowing only a small amount of food to be eaten at once. After the separation of the stomach into a smaller tube, the remainder of the stomach is removed. The valve at the outlet of the stomach (the pylorus) remains in place, which helps to allow for the feeling of fullness.
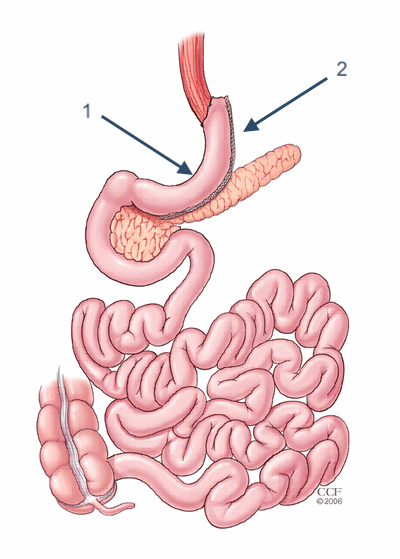
SG is now an established first procedure (or first stage of a two-part surgery) to prepare the obese patient for biliopancreatic diversion or gastric bypass. It is also used as a single-stage procedure. There is no anastomosis or new connections made between the stomach and small intestine in this procedure. There is no rerouting of the intestine. There is no malabsorption. There is no dumping syndrome. The sleeve gastrectomy is believed to have an advantage over other surgeries due to the removal of the part of the stomach that produces the hormone (Ghrelin) that controls hunger and the desire to eat.
The potential complications of the sleeve operation are typically less than those suffered during a gastric bypass or a combined procedure.
Weight loss surgery (bariatric surgery) requires personal responsibility, lifestyle changes, long-term monitoring, and follow-up vitamins.
Studies show that patients that commit to eating healthy food, taking nutritional supplements, and having routine blood work for monitoring purposes have the best long-term results.
Surgery gives patients the physical tool to assist with weight loss. Patients must be committed to making the emotional and physical changes necessary after weight loss surgery. This commitment will ensure successful weight loss and long-term weight maintenance.
Lack of exercise, poorly balanced meals, constant grazing, eating processed foods, and drinking carbonated beverages are some of the most common reasons for weight regain. Good habits of food intake and exercise will need to be practiced for the rest of the patient’s life. This can be viewed as a small commitment when compared to the potential for restored health and improvements or elimination of many of the co-morbidities secondary to obesity.
Why choose the Sleeve Gastrectomy?
The sleeve gastrectomy has the following advantages:
- It does not require the implantation of a foreign body such as that used in gastric banding.
- The procedure mechanically decreases the size of the stomach but also decreases the secretion of the hormone ghrelin which is responsible for the feeling of hunger and satiety (fullness).
- There is no ‘rearranging’ of the intestines so there are no complications of malabsorption such as dumping syndrome.
- Complications secondary to gastric bypass such as marginal ulcer and internal hernia do not occur with this procedure.
- The procedure offers the benefit of initially decreasing the body weight in the severely obese patient to prepare this patient for a staged procedure or other surgery at a later time.